The ethos of the University of Pennsylvania endodontic philosophy is guided by an unceasing assessment of biological mandates that predicate clinical recommendations for predictably successful treatment outcomes. None are more essential than working length determination. And yet, the conclusions derived and recommendations made from the scientific evidence are not in concert with many mainstream endodontic philosophies espoused by leaders in the field.
Where does the root canal space terminate and at what position should the root canal filling be located? Numerous locations have been proposed; 1) the Minor Apical Foramen (MAF), 2) the Apical Constriction (AC), 3) the Radiographic Apex (RA) or Radiographic Terminus (RT), 4), the Major Apical Foramen (MAF) and 5), the Cemento-Dentinal Junction (CDJ) [Fig 1]. From a de facto standpoint, only two of these positions do not vary from tooth to tooth; the Radiographic Apex (RA) and the Cemento-Dentinal Junction (CDJ).
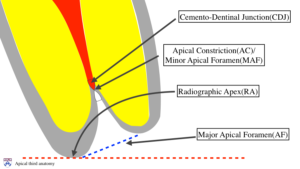
Fig 1
The radiographic apex as a clinically definable terminus is very appealing to techno-clinicians. Filling to the radiographic apex has a “bullseye” aura and like “puffs”, speciously represents the optimal point for root canal space obturation. However; from a biological approach, the bio-clinician recognizes that the root is covered by cementum, indistinguishable from dentin in a radiograph. It is periodontal ligament that forms cementum. Filling to the radiographic apex implies that the “fill” is into the periodontal ligament. This is not a biologically sound terminus and is not supported by the treatment outcomes literature which will be addressed shortly. The Cemento-Centinal Junction is the locus where the root canal ends (dentin produced by pulp) and the periodontal ligament begins (cementum produced by PDL). A biologic approach dictates the root canal fill should culminate at this juncture. This termination position will almost always be short of the radiographic apex due to the cemental cap that is present at the tip of the root. Because we cannot predictably ascertain how short we should fill, techno-clinicians are not attracted to this philosophy.
What do treatment outcome studies suggest? Literally every study concludes that filling short of the radiographic apex results in a greater degree of success than filling long. The classical study by Sjorgren et al (J Endod 1990 Oct;16(10):498-504) has been duplicated many times with essentially the same results. Filling 0-2mm short is best, long is always worse than short and the prognosis decreases as the short fill increases above 2mm [Fig 2].
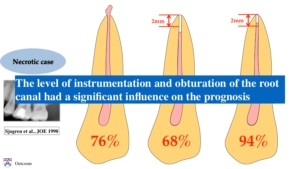
Fig 2
Intriguingly, the optimal filling locus for vital teeth is shown to be 0 – 2mm short of the RA, whereas, for necrotic teeth with apical periodontitis, it is 0.5 – 1mm short of the RA. The techno-clinician incorrectly assumes that this is because in non-vital teeth, we need to get closer to the end of the root to more effectively eradicate microbes. In fact, the correct explanation is that in teeth with apical periodontitis, there is usually resorption of the cementum layer around the apex making the CDJ appear closer to the radiographic apex [Figs 3, 4].
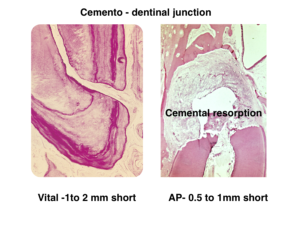
Fig 3
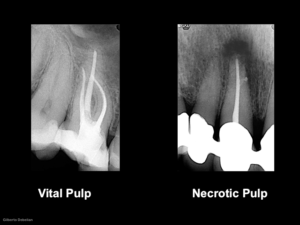
Fig 4
Methods of Working Length Determination: Assessing the correct working length is a differential diagnostic decision using a variety of methods; tactile sense, paper point, radiographs, patient response, average root length, electronic apex locator. The Electronic Apex Locator is considered the most reliable of these methods. Its algorithmic configuration, depending on the generation, uses impedance, resistance, frequency and comparative databases to locate the CDJ. Research shows that if used correctly and if the canal is patient and not blocked with dentinal debris, it does so with amazing accuracy (> 90%). It should be apparent, that a biological approach using outcome studies as our guide, mandates that we fill short of the radiographic apex within a range of 0.5 to 2mm, using an apex locator followed by a pre-root filling check radiograph to assist us in determining the exact length within this range.